Varicose veins of the lower extremities are characterized by the expansion of the superficial veins of the legs, which accompanies the violation of blood flow in them and the failure of the valves. As a result, the veins increase in length and diameter, acquire a serpentine, cylindrical or saccular appearance, although there is also a mixed manifestation of the listed deformities.
Features of the venous system
The emergence and development of varicose veins is directly related to the venous system of the legs, which consists of:
- saphenous veins: small and large;
- deep veins (in the lower leg and thigh);
- perforating veins, which are the connecting link of the two previous systems.
Normally, 90% of blood is transported to the lower extremities through deep veins, and the remaining 10% through superficial ones. When it returns to the side of the heart, this mechanism is supported by valves in the walls of the veins. When the next portion of blood arrives, they slam to prevent its movement from top to bottom under the influence of gravitational force. Muscle contractions push blood further to the heart, allowing normal blood flow.
With a long stay of a person in an upright position, blood stasis may develop, which increases the pressure in the veins and causes an increase in their diameter. This process provokes incomplete closure of the valve leaflets, as a result of which the blood flow is disturbed with its reverse flow from the heart - reflux.
The deep vein valves are most likely to be affected, since they transport the largest amount of blood and therefore experience the maximum load. To lower the high pressure in them, part of the blood is transported by perforated veins to the superficial ones, which were not originally intended for a large volume. Such a load on the walls of the veins leads to their expansion and the formation of varicose veins.
At the same time, blood enters the deep veins without stopping, but due to the violation of their functions and the normal activity of the valve leaflets of the perforated veins, the blood is redistributed to the superficial vessels. As a result of this, chronic varicose veins develops, which over time is accompanied by painful sensations, edema and trophic ulcers.
Causes of the disease
Previously, one of the main causes of varicose veins was called the hereditary factor, but today this theory has been refuted. Of course, it is possible to trace the frequent manifestations of the disease in some families, but this is more likely due to the peculiarities of life that are imparted in the family: food culture, passive rest, sedentary work, and the like.
The development of varicose veins is based on the presence of reflux in the venous system, when blood circulates through the veins in the opposite direction. Additional transportation of blood from deeply located veins to superficial veins is possible due to congenital or acquired degenerative pathology of the valve apparatus. This causes overfilling of superficial vessels with blood and their distension when venous nodes form.
One of the fundamental reasons for the development of varicose veins is considered to be unhealthy diet, which in some cases leads to obesity. Such people move little, mainly eat highly processed foods, and the proportion of plant fiber in the diet is minimized. After all, it is they who are involved in strengthening the walls of veins and blood vessels and prevent prolonged chronic constipation, which greatly increase intra-abdominal pressure and thereby provoke varicose veins. It is noted that an increase in body weight of more than 20% increases the risk of the disease fivefold.
The main provoking factor for women is carrying a child, while the risks of varicose veins increase with each subsequent pregnancy. Severe weight gain and an enlarged uterus put a lot of stress on the legs, which are stagnant. This situation is aggravated by the constantly growing intra-abdominal pressure and the action of the hormone progesterone, which affects the state of elastic fibers in the walls of blood vessels.
Other factors that provoke varicose veins of the lower extremities include:
- a sedentary lifestyle, being upright during the day (such as hairdressers), long flights or long journeys. All this leads to stagnant processes in the lower extremities, when blood accumulates in the superficial veins and is poorly transported towards the heart;
- at times increases the risk of developing varicose veins for women, wearing uncomfortable, tight shoes, especially models with high heels;
- corsets and tight underwear squeeze the inguinal veins and increase intra-abdominal pressure, which is a direct prerequisite for varicose veins;
- high blood pressure;
- smoking, which indirectly leads to a thinning of the walls of blood vessels.
Disease classification
Varicose veins of the lower extremities are classified depending on the prevalence of venous lesions, their localization, as well as the presence of pathological refluxes, which are characterized by impaired blood outflow. There are 4 forms of varicose veins:
- intracutaneous and subcutaneous varicose veins (segmental), in which there is no pathological outflow of venous blood;
- segmental varicose veins, when reflux occurs through perforating or superficial veins;
- a common form of varicose veins, in which reflux occurs through the perforating and superficial veins at the same time;
- varicose veins are characterized by reflux in deep veins.
After the varicose veins of the lower extremities becomes chronic, phlebology considers its three degrees:
- Transient edema, periodically occurring against the background of the syndrome of "heavy legs".
- Persistent, persistent edema. The appearance of hyperpigmentation and eczema is possible.
- Venous ulcer of a trophic nature.
The latter degree is the most difficult to treat, since it requires preliminary removal of inflammation and healing of skin tissues.
Stages and symptoms

The disease develops very slowly, sometimes more than a dozen years pass, until the symptoms that appear will force the patient to seek advice from a phlebologist. At the initial stages of varicose veins, its manifestations are often attributed to fatigue, age, or other reasons. In order to fully consider the symptoms of the disease, its manifestations are classified according to the stages of varicose veins:
- The first stage begins to manifest itself more often at a young age - after 20 years, when there is a feeling of heaviness in the legs, edema may appear, which completely disappear overnight. On the inside of the lower leg, you can see an enlarged vein, which is manifested by a lumpy protrusion of the skin. At this stage, many people notice small spider veins. In general, symptomatology is subtle and rarely gets the attention it deserves.
- The second stage is characterized by an increase in the external manifestation of the dilated vein. The disease is already developing against the background of the pathological work of the venous valves, therefore, the saphenous veins noticeably increase in size, and their lengthening can also be noted. More often there is heaviness and burning in the legs, they quickly get tired with long walks.
- The disease is already becoming chronic due to the constant imbalance in the outflow of venous blood. In the evenings, patients suffer from near-ankle edema, which can be very intense. There is heaviness in the legs, and cramps may occur at night.
- In the absence of treatment in the previous stages, chronic insufficiency of the functioning of the venous system negatively affects the metabolic processes in the skin, the areas in the lower part of the leg are especially affected. Darkening of the skin is visible near the ankle - hyperpigmentation, it thickens and becomes inflamed over time. The described condition is called lipodermatosclerosis. If at this time you do not start therapy with respect to the venous system, then trophic ulcers will soon begin to form.
- The fifth stage is accompanied by numerous trophic ulcers, some of them periodically heal with the formation of scars.
- In the zone of long-standing trophic disturbances, extensive ulcers open. This condition requires urgent active therapy, aimed at both the treatment of varicose veins and the healing of skin ulcers.
Diagnostics
An external examination of the lower extremities in vertical and horizontal positions of the body, palpation of veins and a preliminary assessment of the stage of the disease are carried out. The patient is sent for a general blood test, which allows you to study the picture of the disease with greater thoroughness:
- at the platelet level, a predisposition to thrombosis will be reflected;
- the level of hemoglobin, as well as the number of red blood cells, indicate the degree of blood clotting;
- by the increased level of leukocytes, one can judge about inflammation, which helps to diagnose thrombophlebitis faster.
Be sure to examine the venous system of the legs, for which there are many methods:
- ultrasound dopplerography - ultrasonic scanning;
- phlebography;
- CT phlebography;
- duplex angioscanning - USAS;
- phleboscintiography;
- photoplesmography;
- phlebomanometry and the like.
In practice, patients are more often prescribed USAS and USG, as they help to fully study the venous system of the legs and identify degenerative areas. The rest of the methods can be prescribed additionally if the ultrasound examination did not give a complete vision of the picture of the disease. Some of these methods can have complications such as venous thrombosis, perforation of the vessel wall with a catheter, and allergy to contrast agent. Consider the most commonly practiced techniques in phlebology:
- USAS allows assessing the anatomical, hemodynamic and functional pathologies of the venous bed. The data obtained are subject to computer processing, after which a model of the venous system can be viewed on video or printed on paper.
- Doppler ultrasound with high accuracy determines the patency of superficial and deeply located veins, blood flow velocity. Doppler ultrasonography makes it possible to assess the functioning of the valve apparatus.
After extensive diagnostics, the doctor draws up a patient's phlebocard, which allows you to determine the damaged segments of the venous system, their degree and length. After that, a suitable treatment is selected.
Treatment
It is carried out in a comprehensive manner and is determined based on the symptoms, the degree of development of the disease and the results of the study. In the initial stages, conservative therapy is prescribed, which consists of:
- Drug treatment when a group of drugs is prescribed:
- antioprotectors and phlebotonics;
- anticoagulants;
- disaggregants
- topical preparations (ointments, gels);
- anti-inflammatory drugs.
- Elastic compression, for which compression hosiery or bandaging is used (rarely). It allows you to dose the squeezing of muscles, prevents stagnant processes, and improves blood flow through the vessels. When wearing such underwear, there is an effect of artificially maintaining vascular tone.
- Physiotherapeutic methods, among which the best treatment results were shown by electrophoresis, diadynamic currents, laser radiation and a magnetic field.
- Feasible physical activity, which should be performed only in compression underwear (except for swimming). Cycling, swimming, jogging are recommended. The phlebologist selects an individual set of exercises for the lower extremities, which will train the vessels of the legs every day.
In addition, patients are advised to carry out contrasting five-minute procedures in the shower every evening, alternately switching from warm to cold water. Such manipulations improve blood flow and tone blood vessels.
It is important at the beginning of treatment to identify the disease-provoking factor in order to effectively influence it. And patients who are at risk should visit a phlebologist every 2 years for a preventive examination and do an ultrasound examination of the veins in the legs.
When conservative treatment does not give results or varicose veins are observed at an advanced stage, then surgical intervention is used. Today varicose veins can be completely cured thanks to the following methods:
- Phlebectomy. The essence of the operation is to remove the main trunks of the superficial vein to eliminate the pathological discharge of blood. Perforating veins are often ligated for the same purpose.
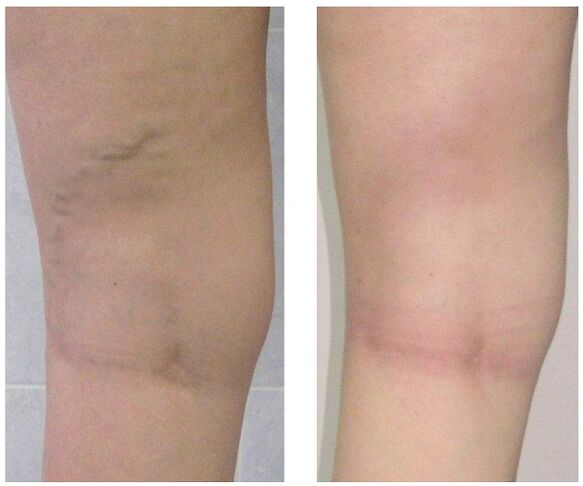
- Sclerotherapy. It consists in the introduction of a sclerosant into the affected area of the vein, which leads to the connection of its walls. Recently, they began to actively use for the same purposes foamed sclerosant according to the technology -. The blood flow through the defective area stops and the cosmetic defect in the form of protruding nodules is eliminated. After such an intervention, no scars remain, all manipulations are performed on an outpatient basis without a subsequent inpatient stay. But sclerotherapy is used only for the fusion of small branches of the venous trunks.
- Laser coagulation. With the help of a laser beam, the marked area of the vein is heated, the walls of which stick together and blood flow through it stops. But this technique is indicated only for veins with an expansion diameter of less than a centimeter.
Prevention
Preventive measures can be both primary, aimed at preventing the development of varicose veins, and secondary, when it is required to reduce the risk of recurrence after surgery or prevent the aggravation of the course of the disease. Helpful hints:
- lead an active lifestyle without heavy load on your legs: swimming, walking, cycling;
- watch your weight;
- keep both legs raised more often;
- do not wear tight underwear and heels above 4 centimeters;
- use orthopedic insoles;
- take a contrast shower;
- do five-minute preventive leg exercises daily;
- wear compression stockings for long walks.
If you notice the slightest suspicion of varicose veins - prominent nodules on the legs, swelling, heaviness, then do not postpone a visit to the phlebologist. Indeed, over time, this insidious disease can provoke a lot of complications, including thrombophlebitis and thrombosis.























